The Indispensable Role and Importance of Industry Regulations and Standards in Clinical Trials

Clinical trials are the cornerstone of medical advancement, serving as the crucible where new drugs, therapies, and medical devices are rigorously tested for safety and efficacy. However, these trials' ethical and scientific integrity relies heavily on a robust framework of industry regulations and standards. These guidelines govern every facet of clinical research, from the recruitment and treatment of study participants to data collection and analysis. To learn the nuances of clinical research, you can our Clinical research certification course and get placed in healthcare industry.
In this context, this discussion explores why industry regulations and standards for clinical trials are not just essential but crucial, delving into the profound impact they have on patient welfare.
In the previous blog, we discussed the importance of clinical research processes. Now, we shall discuss the standards of clinical trials in detail.
Every trial stage has to be approved and carried out in regulatory compliance to comply with GCP requirements. The clinical trial requirements may differ by country.
The International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) and the US Food and Drug Administration (FDA) have substantial regulatory weight.
The primary responsibility of public regulation is to ensure that pharmaceutical companies adhere to statutes. Those who interested in drug safety and pharmaceutical practices, can join drug safety and pharmaceutical training.
The statute or regulation requires that discovered drugs be tested, trialed, and manufactured according to the guidelines. If the drug meets these criteria, it implies that it is safe for patients and protects their well-being.
In monitoring the regulatory process, Regulatory authorities should be vigilant in ensuring whether animal studies comply with Good Laboratory Practice (GLP), clinical trials are executed by Good Clinical Practice (GCP), and drugs are discovered under the Good Manufacturing Practice (cGMP) conditions.
The acronym "ICH" represents the "International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use."
ICH is a Collaborative effort that includes research-based industry, regulators, and representatives of Japan, the US, and the EU. These representatives focus on the scientific and technical assessment and testing processes required to assess the safety, quality, and efficacy of medicines.
The International Council on Harmonization (ICH) aims to enhance global uniformity of technical standards to guarantee the safe, efficient, and high-quality development and registration of medicines in the most economical way possible.
There are four main categories into which the ICH Topics fall
♦ Quality (Q): This process ensures the QA process of pharmaceutical and chemical.
♦ Safety (S): Those pertaining to preclinical in vitro and in vivo research
♦ Efficacy (E): Those that deal with clinical research involving human subjects.
♦ Multidisciplinary topics (M): Subjects that don't fit under one of the abovementioned groups.
Efficacy Topics
♦ E3: Structure and Content of Clinical Study Reports
♦ E4: Dose-Response Information to Support Drug Registration
♦ E6: Good Clinical Practice: Consolidated Guideline
♦ E8: General Considerations for Clinical Trials
♦ E9: Statistical Principles for Clinical Trials
♦ E10: Choice of Control Group and Related Issues in Clinical Trials
The International Council on Harmonization (ICH) aims to provide suggestions for a more uniform interpretation and implementation of technical guidelines and requirements for registering pharmaceutical products.
Six parties are represented on the ICH Steering Committee and its subcommittee, which comprises representatives from the research-based industry and regulatory agencies in the USA, EU, and Japan.
Region- Japan
Regulatory Body - MHLW - Ministry of Health, Labour and Welfare
Research-Based Industry- JPMA-Japan Pharmaceutical Manufacturers Association
Region - Europe
Regulatory Body- EU - European Union
Research-Based Industry- EFPIA - European Federation of Pharmaceutical Industries and Associations
Region - USA
Regulatory Body - FDA - Food and Drug Administration
Research-Based Industry - PhRMA - Pharmaceutical Research and Manufacturers of America
U.S.FDA: The U.S. FDA, or United States Food and Drug Administration, is the U.S. Department of Health and Human Services (HHS) federal agency. The FDA protects and promotes public health by regulating and supervising various products and industries related to food safety, pharmaceuticals, medical devices, biologics, cosmetics, and more.
21 CFR Part 11 Compliance: 21 CFR Part 11 is a regulation issued by the United States Food and Drug Administration (FDA) that sets forth requirements for electronic records and electronic signatures in the context of FDA-regulated industries, particularly pharmaceuticals, biotechnology, and medical devices. Compliance with 21 CFR Part 11 is essential for organizations dealing with electronic records and signatures.
Title 21 of the Code of Federal Regulations (CFR)
Parts applicable to clinical research
Part 11 - Electronic Records and Signatures
Part 50 - Protection of Human Subjects
Part 54 - Financial Disclosure by Clinical Investigators Part 56 - Institutional Review Boards
Part 312 - Investigational New Drug Application
Part 314 - Applications for FDA Approval to Market a New Drug or an Antibiotic Drug
Part 600 - Biological Products
Part 812 - Medical Devices
Departments and Roles in a CRO
Contract Research Organization: A Contract Research Organization (CRO) is a specialized service provider that assists pharmaceutical, biotechnology, and medical device companies in conducting clinical trials and research. Within a CRO, various departments and roles collaborate to ensure the successful planning, execution, and monitoring of clinical studies.
A typical clinical research organization includes the following departments:
Clinical Operations
Regulatory Affairs
Data Management and Biostatistics
Medical and Scientific Affairs
Quality Assurance (QA) and Compliance
Project Management
Business Development
Finance and Administration
Safety and Pharmacovigilance
Clinical Laboratories
Clinical Supplies and Logistics
Each department and role within a CRO plays a vital role in the comprehensive and successful execution of clinical trials. Together, they contribute to developing safe and effective medical treatments and therapies that benefit patients and advance the healthcare industry.
Key Functions in Clinical Operations
Clinical Operations professionals are involved in the initial planning of clinical trials. This includes protocol development, feasibility assessments, site selection, and determining the overall study strategy.
Site Managers often visit clinical sites to monitor progress and compliance with the protocol.
They ensure the study is conducted according to the protocol, Good Clinical Practice (GCP) guidelines, and regulatory requirements.
They ensure data quality, accuracy, and integrity throughout the trial.
Clinical Operations professionals prepare and submit regulatory documents, manage inspections, and address compliance issues.
Clinical Operations is responsible for the closeout process, including site closeout visits, final data collection, and archiving of trial documentation.
Support Investigator as and when required (e.g., Finalization of Investigator agreements and contracts, Finalization of Protocol and CRF)
Key Functions in Data Management
1. Data Collection
2. Data Storage
3. Data Cleaning
4. Data Integration
5. Data Transformation
6. Data Analysis
7. Data Visualization
8. Data Security
9. Data Governance
10. Data Archiving
Protocol: Clinical research will start after the plan is formulated. The plan covers the start to end point of the clinical research. Moreover, the plan describes what should focus on the study, how it can conduct, and why each part of studies is crucial. The protocol or plan is designed to protect the participant's health and answer distinctive research questions.
Case Report Form (CRF):
The Case Report Form (CRF) is a meticulously designed tool in clinical research that is pivotal for gathering structured and standardized data from study participants. CRFs serve as an essential documentation source, enabling transparent reporting, informed decision-making, and the generation of robust evidence to evaluate the safety and efficacy of investigational products, ultimately advancing medical research and patient care.
To learn clinical data management, its significance, and the role of data managers in clinical trials. you can enroll in Clinical Data Management training.
Key Functions in Quality Assurance
Prepare and distribute quality reports to management and stakeholders to communicate performance, trends, and improvement areas.
Providing training to employees to ensure they have the necessary skills and knowledge to perform their roles effectively and maintain quality standards.
They collaborate with external vendors, such as central laboratories and imaging facilities, to ensure the timely and accurate delivery of services required for the trial.
Ensure the director of quality assurance and medical affairs is notified of any problems with GCP compliance at sites or elsewhere.
Maintaining version control of SOPs ensures that all employees adhere to the most recent and accurate SOP instructions or guidelines.
Functions in Pharmacovigilance
Collaboration between regulatory authorities, pharmaceutical companies, and healthcare organizations worldwide to share safety data, harmonize reporting standards, and develop global strategies for risk management.
Ensuring that clinical trials conducted in multiple countries adhere to uniform safety monitoring and reporting standards, allowing for the global evaluation of a product's safety profile.
ADR information informs product labeling and patient information leaflets. It helps healthcare professionals and patients understand potential risks associated with a product, enabling safer use.
By analyzing ADR data, pharmacovigilance contributes to continuous improvement in the safety of healthcare products.
Key Functions in Medical Writing
Clinical Study Documents
Regulatory Submissions
Managing SAEs during clinical trials
Clinical Study Reports (CSRs)
Manage SAEs during clinical trials
Adherence to Ethical Guidelines
Writing Medical Cases
Closely involved in the regulatory department's narrative preparation for submissions.
Standard Operating Procedure (SOP): A Standard Operating Procedure (SOP) is a documented, step-by-step set of guidelines and instructions that outlines the standardized procedures and processes to be followed in an organization's specific task or activity.
Adverse Drug Reaction (ADR): An Adverse Drug Reaction (ADR) is an unintended and harmful response or side effect caused by a pharmaceutical product, such as a drug, vaccine, or medical device.
Serious Adverse Event (SAE): A Serious Adverse Event (SAE) is a significant and severe medical occurrence or outcome resulting from the use of a medical product, often requiring hospitalization, posing a life-threatening risk, causing persistent disability, congenital anomalies, or resulting in death.
In conclusion, industry regulations and standards for clinical trials play a fundamental role in safeguarding research integrity, safety, and ethical conduct. These rigorous guidelines ensure that new treatments and therapies are developed with precision, transparency, and patient well-being. Adherence to these regulations not only fosters public trust but also advances the pursuit of groundbreaking medical discoveries that have the potential to transform healthcare.
Find a course provider to learn Clinical Research
Java training | J2EE training | J2EE Jboss training | Apache JMeter trainingTake the next step towards your professional goals in Clinical Research
Don't hesitate to talk with our course advisor right now
Receive a call
Contact NowMake a call
+1-732-338-7323Enroll for the next batch
Clinical Research Training Course Program
- Dec 17 2025
- Online
Clinical Research Training Course Program
- Dec 18 2025
- Online
Clinical Research Training Course Program
- Dec 19 2025
- Online
Related blogs on Clinical Research to learn more

CDISC SDTM: Standardizing Clinical Data for Enhanced Research Insights
Learn the importance of CDISC SDTM standards in enhancing research insights by standardizing clinical data.

Exploring the Significance of Medical History in Healthcare
Discover the crucial role of medical history in healthcare, understanding how it informs diagnosis, treatment, and patient care, and its impact on the evolution of medicine.
Key Stages of a Typical Clinical Trial Process Flow
Clinical trials follow a well-defined process flow that is essential for conducting successful and ethical clinical research.

Understanding the Key Stages of a Typical Clinical Trial Process Flow
Discover the critical steps involved in each stage, ensuring a smooth and successful clinical trial process flow.
Unveiling the Clinical Research Roadmap: A Comprehensive Guide
We have discussed the purpose of Clinical research processes, and what is clinical research process.
Corona Virus (COVID-19), Symptoms, Tests and Safety Measures
Corona Virus (COVID-19), Symptoms, Tests and Safety Measures. Learn the symptoms, tests to undergo, and safety measures to be taken to prevent the virus.

List of Best Clinical Research Training in Atlanta – CRC, CRA, MSCR Studies
We have collected a list of reputed institutes to those interested in pursuing a career in clinical and/or translational research. Pick from the list to have your dream come true career in medicine.

Healthcare Sector increasing the focus in Big Data and Technology
Here the role of technology business mergers and big data firms within the healthcare frontiers comes into play. The business mergers of technology, as well as the big data firms in the healthcare sector, highlights a trend viral within the clinical

7 Ethics for Clinical Researchers
Clinical trials conducted by the researchers involve a human volunteer who is willing to be subject to adhere new findings or a medical experiment. For that, a proper consent is acquired from the volunteer before conducting the trials.

Will lowering Blood Pressure would save lives? Clinical Trials Says so…
So far, the healthcare industry had been advised that the blood pressure of a healthy adult has to be less than 140 millimeters of mercury. And any increase in blood pressure that this guideline would attract serious consequences such as heart attack
Latest blogs on technology to explore
From Student to AI Pro: What Does Prompt Engineering Entail and How Do You Start?
Explore the growing field of prompt engineering, a vital skill for AI enthusiasts. Learn how to craft optimized prompts for tools like ChatGPT and Gemini, and discover the career opportunities and skills needed to succeed in this fast-evolving indust

How Security Classification Guides Strengthen Data Protection in Modern Cybersecurity
A Security Classification Guide (SCG) defines data protection standards, ensuring sensitive information is handled securely across all levels. By outlining confidentiality, access controls, and declassification procedures, SCGs strengthen cybersecuri

Artificial Intelligence – A Growing Field of Study for Modern Learners
Artificial Intelligence is becoming a top study choice due to high job demand and future scope. This blog explains key subjects, career opportunities, and a simple AI study roadmap to help beginners start learning and build a strong career in the AI
Java in 2026: Why This ‘Old’ Language Is Still Your Golden Ticket to a Tech Career (And Where to Learn It!
Think Java is old news? Think again! 90% of Fortune 500 companies (yes, including Google, Amazon, and Netflix) run on Java (Oracle, 2025). From Android apps to banking systems, Java is the backbone of tech—and Sulekha IT Services is your fast track t
From Student to AI Pro: What Does Prompt Engineering Entail and How Do You Start?
Learn what prompt engineering is, why it matters, and how students and professionals can start mastering AI tools like ChatGPT, Gemini, and Copilot.

Cyber Security in 2025: The Golden Ticket to a Future-Proof Career
Cyber security jobs are growing 35% faster than any other tech field (U.S. Bureau of Labor Statistics, 2024)—and the average salary is $100,000+ per year! In a world where data breaches cost businesses $4.45 million on average (IBM, 2024), cyber secu

SAP SD in 2025: Your Ticket to a High-Flying IT Career
In the fast-paced world of IT and enterprise software, SAP SD (Sales and Distribution) is the secret sauce that keeps businesses running smoothly. Whether it’s managing customer orders, pricing, shipping, or billing, SAP SD is the backbone of sales o

SAP FICO in 2025: Salary, Jobs & How to Get Certified
AP FICO professionals earn $90,000–$130,000/year in the USA and Canada—and demand is skyrocketing! If you’re eyeing a future-proof IT career, SAP FICO (Financial Accounting & Controlling) is your golden ticket. But where do you start? Sulekha IT Serv

Train Like an AI Engineer: The Smartest Career Move You’ll Make This Year!
Why AI Engineering Is the Hottest Skillset Right Now From self-driving cars to chatbots that sound eerily human, Artificial Intelligence is no longer science fiction — it’s the backbone of modern tech. And guess what? Companies across the USA and Can
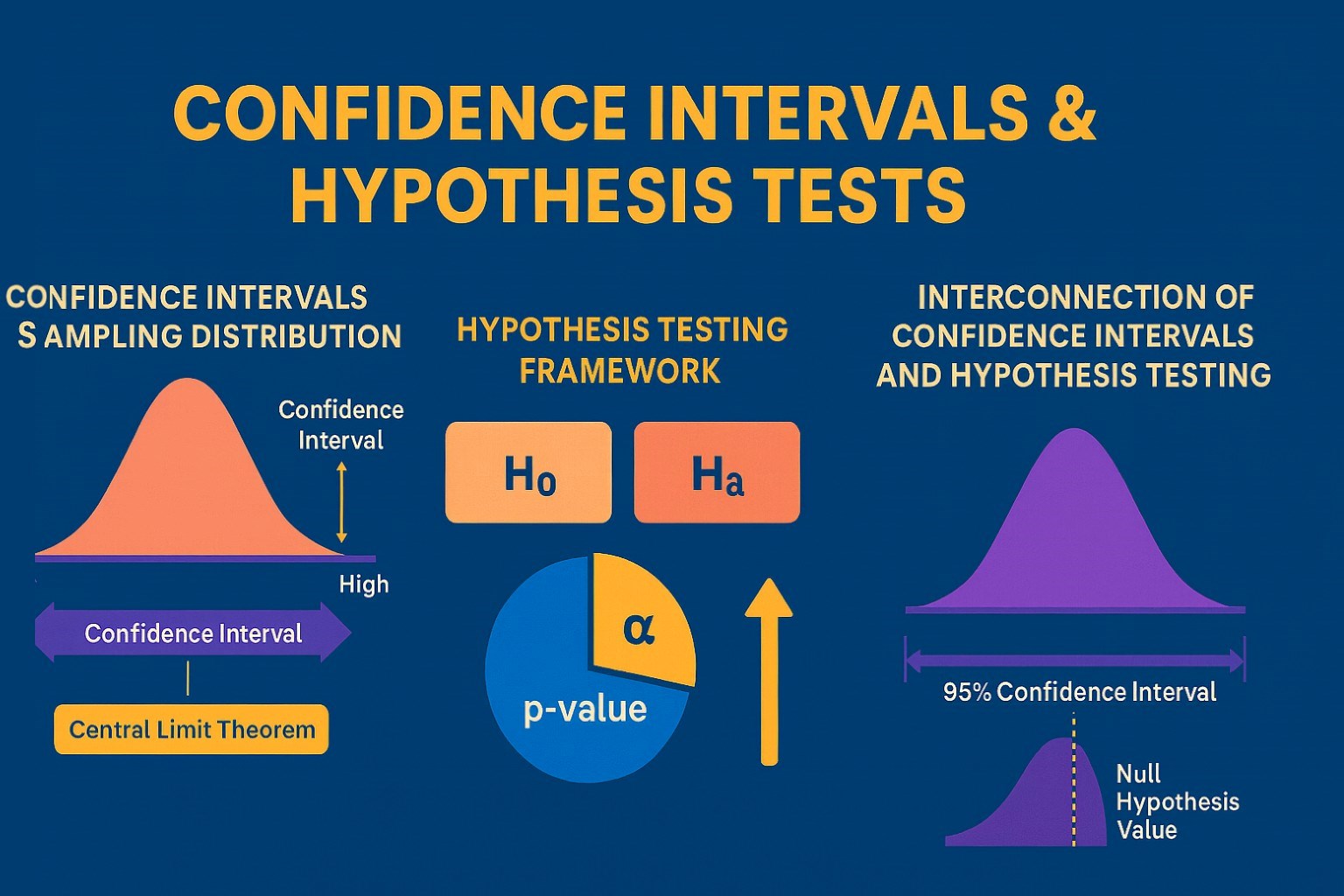
Confidence Intervals & Hypothesis Tests: The Data Science Path to Generalization
Learn how confidence intervals and hypothesis tests turn sample data into reliable population insights in data science. Understand CLT, p-values, and significance to generalize results, quantify uncertainty, and make evidence-based decisions.