What is QNXT in Healthcare?

QNXT has gained significant demand in the healthcare industry due to its robust and comprehensive features tailored to meet the complex needs of health plans and payers. As healthcare administration becomes increasingly intricate, organizations seek solutions to streamline processes and enhance operational efficiency. QNXT addresses these challenges by offering a versatile platform for claims processing, enrollment, billing, care management, and more.
With integration capabilities, reporting tools, and a focus on compliance, QNXT enables health plans to navigate the evolving healthcare landscape, improve member services, and stay ahead in an industry that demands agility, precision, and regulatory standards.
What is QNXT in healthcare?
QNXT is a comprehensive core administration system designed for the healthcare industry, offering a range of features to streamline and optimize essential processes. Developed by HealthEdge, this platform is tailored for health plans and payers, providing robust capabilities in claims processing, enrollment and eligibility management, billing and invoicing, care management, and utilization management. One of its key strengths lies in its configuration and customization, allowing healthcare organizations to adapt the system to their specific workflows.
QNXT facilitates efficient provider network management, integrates with other healthcare systems for seamless data exchange, and incorporates reporting and analytics tools for data-driven decision-making. This solution aims to enhance operational efficiency, improve member services, and ensure compliance with the complex regulatory landscape of the healthcare sector.
Who Uses QNXT?
QNXT is widely adopted by:
1. Health Plans for managing diverse lines of business like Medicaid, Medicare, and Commercial insurance.
2. Third-Party Administrators (TPAs) for streamlined claims and provider network management.
3. Integrated Delivery Networks (IDNs) to consolidate and optimize healthcare processes.
4. Government-Sponsored Programs for compliance-driven administrative tasks.
Now, we shall discuss the key features of QNXT in healthcare.
QNXT Key Features:
1. Claims Processing Excellence:
- QNXT excels in end-to-end claims processing, providing a streamlined workflow for accurate and timely claims management.
2. Enrollment and Eligibility Mastery:
- Managing member enrollment and eligibility is seamless with QNXT, ensuring health plans have up-to-date and accurate member data.
3. Billing and Invoicing Efficiency:
- The platform supports billing and invoicing processes, enabling health plans to manage financial transactions and revenue cycles with precision.
4. Care Management Optimization:
- QNXT contributes to effective care management, helping health plans coordinate and optimize healthcare services for their members.
5. Configurability and Customization:
- Recognizing the diverse needs of healthcare organizations, QNXT offers configuration and customization, allowing adaptation to specific workflows.
6. Integration Capabilities:
- QNXT seamlessly integrates with other healthcare systems and external partners, facilitating smooth data exchange and interoperability.
7. Utilization Management Support:
- The platform assists in utilization management, enabling organizations to assess and ensure the appropriateness of healthcare services.
8. Provider Network Management:
- QNXT helps maintain accurate and up-to-date information about healthcare providers, contributing to effective provider network management.
9. Reporting and Analytics Tools:
- With robust reporting and analytics tools, QNXT empowers health plans with insights into key performance indicators, supporting data-driven decision-making.
Custom Reporting Dashboards
10. Custom Reporting Dashboards
Customizable dashboards allow organizations to track key metrics, such as claims processing time, financial performance, and regulatory compliance.
QNXT Benefits and Impact:
Health plans choose QNXT for its ability to enhance operational efficiency, improve member services, and ensure compliance with the intricate regulatory landscape of the healthcare industry. The platform's demand stems from its adaptability to various workflows, scalability to meet the evolving needs of organizations, and its role as a strategic asset in navigating the complexities of modern healthcare administration. In essence, QNXT stands as a transformative force, empowering health plans to thrive in an industry that demands agility, accuracy, and a commitment to delivering high-quality care.
How QNXT Workflow Streamline critical business processes
1. It helps reduce costs
2. Improve operational efficiency
3. Increase automation
4. Has a rich set of easily configurable modules for payers
5. Aid in providing productivity and performance
6. Help reduce administrative costs and overall TCO
7. Improve member and provider experiences
8. Help meet their business needs across multiple lines of business on a single platform
These are the enhanced features and functionality to optimize your operations. Moreover, this helps prioritize, triage, and reduce pending and exception claims and utilize management inventory, appeals & grievances tasks.
TriZetto® QNXT™ Healthcare Workflow Solutions
TriZetto® QNXT™ Claims Workflow- This is a part of the QNXT software platform that manages the entire lifecycle of a healthcare claim, from submission to payment.
TriZetto® QNXT™ Utilization Management Workflow- It helps track pre-authorization requests and medical necessity reviews and ensure that treatments meet the standards of care.
TriZetto® QNXT™ Appeals and Grievance Workflow- The appeals and grievance workflow tracks the progress of appeals, documents communications, and ensures compliance with regulatory requirements.
Comprehensive QNXT™ and TriZetto® Solutions for Healthcare Administration:
QNXT™ Workflow- Automates and manages administrative processes such as claims, authorizations, and member enrollment.
QNXT™ Open Access- Provides flexibility for healthcare providers and patients, allowing easier access to care without pre-authorization in open-access health plans.
QNXT™ DOFR Module- Manages financial responsibility between payers and providers, ensuring clear payment guidelines.
QNXT™ Dental Module- Specializes in dental benefits management, claims processing, and provider handling for dental care.
TriZetto® Robotic Process Automation- Automates repetitive tasks using bots, improving efficiency and reducing errors in healthcare workflows.
TriZetto® QNXT™ Solutions
TriZetto QNXT Core Administration System- The main platform for managing healthcare administration processes
TriZetto® myQNXT Dashboard- A customizable dashboard that provides real-time insights and helps manage daily tasks
TriZetto® myQNXT™ Successful daily interactions start with a streamlined digital workspace- A centralized workspace designed for efficient daily healthcare operations.
TriZetto® QNXT-based solutions for Medicaid- Solutions tailored for managing Medicaid programs and ensuring compliance with state and federal requirements.
Main modules in QNXT and their functionalities
Claims Management Module
Member Management Module
Billing and Premium Management Module
Provider Management Module
Utilization Management Module
Appeals and Grievances Module
Financial Management Module
Reporting and Analytics Module
Billing and Premium Management Module
Other services
Business process services
Business Consulting
Next-gen technologies
Infrastructure services
IT professional services
Services/Benefits administration
Business process-as-a-service
Why is QNXT the Future of Healthcare Administration?
1. Data-Driven Insights: Its analytics capabilities provide actionable insights to improve care quality and operational efficiency.
2. Cloud-Based Flexibility: Many organizations are moving their QNXT systems to the cloud, ensuring 24/7 accessibility and scalability.
3. AI-Powered Optimization: Leveraging artificial intelligence, QNXT improves decision-making and automates repetitive tasks.
4. Member-Centric Focus: QNXT supports personalized member portals, enhancing engagement and satisfaction.
Examples of Use Cases
Large Health Plans: Streamlining operations for millions of members.
Medicaid Programs: Ensuring compliance with state and federal guidelines.
Small Providers: Cost-effective solutions for billing and claims management.
Why Choose QNXT Over Competitors?
1. Comprehensive Ecosystem: QNXT covers a wider range of healthcare processes than most competitors.
2. AI-Powered Automation: Reduces manual intervention, improving accuracy and efficiency.
3. Scalability for Growth: Supports organizations as they expand, ensuring seamless upgrades.
4. Integration-Friendly: Easily connects with EHRs, CRM tools, and other healthcare platforms.
5. Dedicated Support: Offers extensive training resources and 24/7 support for healthcare providers.
Frequently Asked Questions About QNXT
1. Can QNXT support small healthcare organizations?
Yes, QNXT is highly scalable and offers customizable modules to fit the needs of both small and large organizations.
2. Is QNXT compliant with the latest healthcare regulations?
Absolutely. QNXT is regularly updated to comply with regulations like HIPAA, ICD-10, and value-based care models.
3. What industries benefit the most from QNXT?
While primarily used in healthcare, QNXT's flexibility makes it valuable for government-sponsored programs, TPAs, and integrated delivery networks.
Find a course provider to learn QNXT Claims Processing System
Java training | J2EE training | J2EE Jboss training | Apache JMeter trainingTake the next step towards your professional goals in QNXT Claims Processing System
Don't hesitate to talk with our course advisor right now
Receive a call
Contact NowMake a call
+1-732-338-7323Enroll for the next batch
QNXT Claims Processing System
- Dec 10 2025
- Online
QNXT Claims Processing System
- Dec 11 2025
- Online
QNXT Claims Processing System
- Dec 12 2025
- Online
Latest blogs on technology to explore
From Student to AI Pro: What Does Prompt Engineering Entail and How Do You Start?
Explore the growing field of prompt engineering, a vital skill for AI enthusiasts. Learn how to craft optimized prompts for tools like ChatGPT and Gemini, and discover the career opportunities and skills needed to succeed in this fast-evolving indust

How Security Classification Guides Strengthen Data Protection in Modern Cybersecurity
A Security Classification Guide (SCG) defines data protection standards, ensuring sensitive information is handled securely across all levels. By outlining confidentiality, access controls, and declassification procedures, SCGs strengthen cybersecuri

Artificial Intelligence – A Growing Field of Study for Modern Learners
Artificial Intelligence is becoming a top study choice due to high job demand and future scope. This blog explains key subjects, career opportunities, and a simple AI study roadmap to help beginners start learning and build a strong career in the AI
Java in 2026: Why This ‘Old’ Language Is Still Your Golden Ticket to a Tech Career (And Where to Learn It!
Think Java is old news? Think again! 90% of Fortune 500 companies (yes, including Google, Amazon, and Netflix) run on Java (Oracle, 2025). From Android apps to banking systems, Java is the backbone of tech—and Sulekha IT Services is your fast track t
From Student to AI Pro: What Does Prompt Engineering Entail and How Do You Start?
Learn what prompt engineering is, why it matters, and how students and professionals can start mastering AI tools like ChatGPT, Gemini, and Copilot.

Cyber Security in 2025: The Golden Ticket to a Future-Proof Career
Cyber security jobs are growing 35% faster than any other tech field (U.S. Bureau of Labor Statistics, 2024)—and the average salary is $100,000+ per year! In a world where data breaches cost businesses $4.45 million on average (IBM, 2024), cyber secu

SAP SD in 2025: Your Ticket to a High-Flying IT Career
In the fast-paced world of IT and enterprise software, SAP SD (Sales and Distribution) is the secret sauce that keeps businesses running smoothly. Whether it’s managing customer orders, pricing, shipping, or billing, SAP SD is the backbone of sales o

SAP FICO in 2025: Salary, Jobs & How to Get Certified
AP FICO professionals earn $90,000–$130,000/year in the USA and Canada—and demand is skyrocketing! If you’re eyeing a future-proof IT career, SAP FICO (Financial Accounting & Controlling) is your golden ticket. But where do you start? Sulekha IT Serv

Train Like an AI Engineer: The Smartest Career Move You’ll Make This Year!
Why AI Engineering Is the Hottest Skillset Right Now From self-driving cars to chatbots that sound eerily human, Artificial Intelligence is no longer science fiction — it’s the backbone of modern tech. And guess what? Companies across the USA and Can
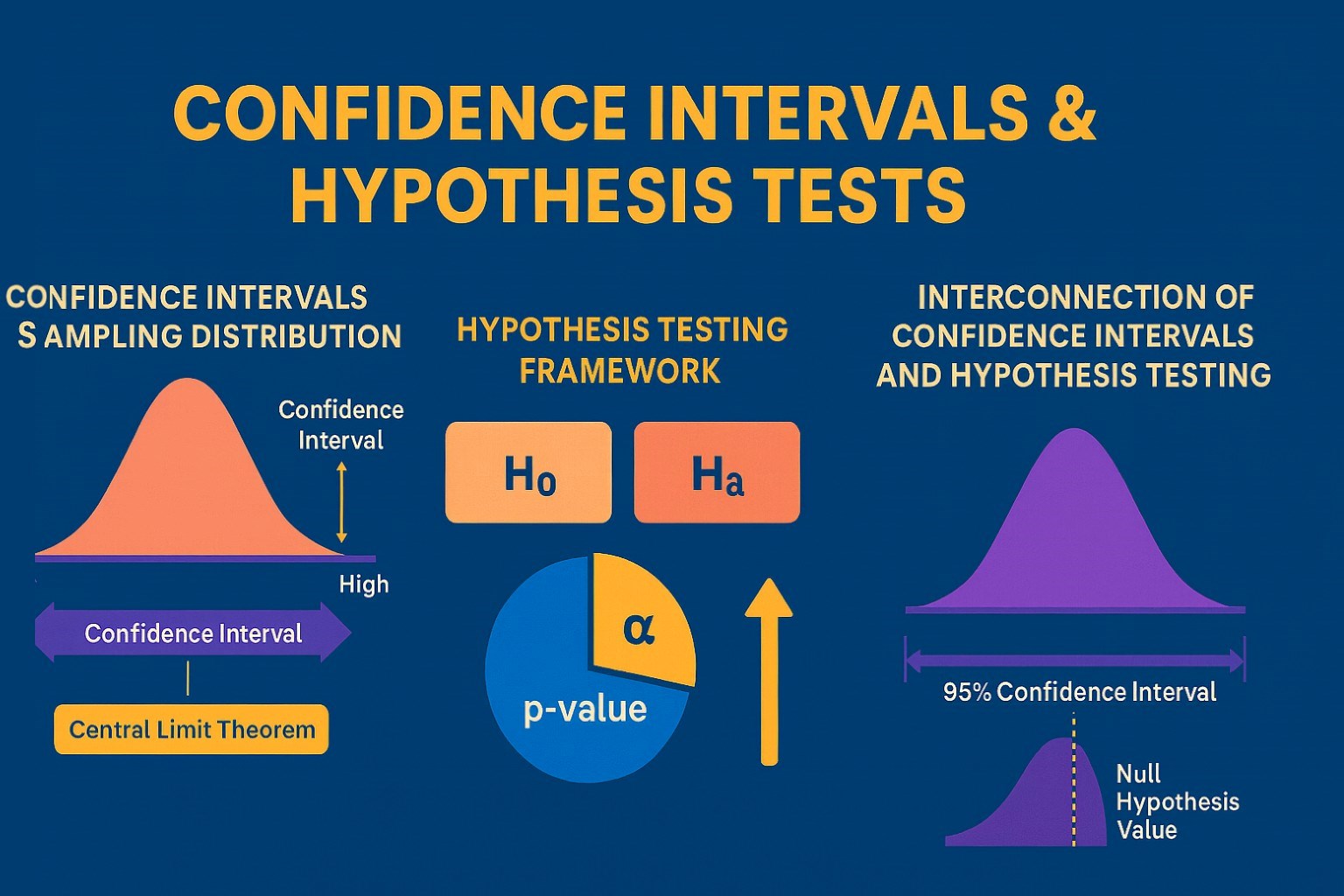
Confidence Intervals & Hypothesis Tests: The Data Science Path to Generalization
Learn how confidence intervals and hypothesis tests turn sample data into reliable population insights in data science. Understand CLT, p-values, and significance to generalize results, quantify uncertainty, and make evidence-based decisions.