What is FACETS in healthcare?

Facets is a healthcare administration software developed by TriZetto, designed for insurance payers and health plans to manage core operations like member enrollment, claims processing, billing, provider network management, and care coordination. It helps healthcare organizations automate workflows, adapt to regulatory changes, and deliver secure, personalized services efficiently. Facets enables payers to respond to evolving industry demands without system limitations.
Moreover, FACETS is a solution that helps healthcare plans and adapt to new trends without system limitations. In healthcare, we must pay, make contract arrangements, provide security and personalized health information, and face challenges. In all of these, FACETS plays a crucial role in embracing new changes quickly and efficiently.
In this blog, we shall discuss FACETS, a healthcare administration platform by TriZetto, how used for member enrollment, claims processing, and provider network management. The blog highlights FACETS' key features like automation, analytics, compliance, and integration, benefiting payers, pharmacy benefit managers, and providers. Moreover, we have discussed real-world examples showcase its role in enhancing efficiency, reducing costs, and driving growth in the healthcare sector.
Position your organization for growth and success.
FACETS provides the best solution for the next generation as it integrates consumer, claims, care, and revenue management in a single flexible platform.
Due to its flexibility in features and services, it is trusted by 80+ healthcare organizations worldwide. Facets Core Administration platform has a rich set of functional modules that help payer organizations meet their business requirement and make necessary growth.
Moreover, the transaction process can be easier because Facets addresses the diverse needs of Commercial Groups, Individuals, Managed Medicaid, Medicare Advantage, and Part D and Specialty health plans.
Furthermore, due to its rich ecosystem, many top companies utilize TriZetto Healthcare Products and third-party applications that extend its features and functions.
With Facets, payers can meet the demands of the market by:Payer organizations can enable next-generation servicesWith this, we can achieve the next level of productivity, enhancement, and performance. Can able to reduce the administrative costsEnhancing the experience for providers and membersAdapting to ever-changing compliance requirements
Who uses FACETS in healthcare?
Currently, FACETS is used by over 540 businesses, 87% of which are US-based. 19% of all the businesses utilizing TriZetto FACETS are small, meaning they employ less than 50 people; 42% are medium-sized; and 38% are large, meaning they employ more than 1000 people. Upon further examination, a large number of the businesses utilizing this IT platform are associated with the following sectors:
- Computer Software (26%)
- Insurance (10%)
- Information Technology and Services (15%)
- Hospital & Health Care (20%)
Regarding the healthcare industry, FACETS serves three main segments:
- Payers
- Pharmacy benefit managers
- Providers
Payers
Payers are businesses like UnitedHealth Group, Anthem, or Cigna that cover the cost of medical services.
Payers need to restructure their businesses to adapt to the changing needs of the healthcare industry if they want to succeed. These demands include new treatment and payment models, incentive realignment, and the quick development of digital technology. FACETS is a digital healthcare service that aids in client engagement and retention for payers.
Pharmacy benefit managers
Pharmacy benefit managers (also called PBMs) aid in managing medical prescriptions on behalf of health insurers, Medicare Part D drug plans, large employers, and other payers.
The development of the digital era has introduced competition that poses a potential challenge to the operations and value proposition of pharmacy benefit managers (PBMs). FACETS enables pharmacy benefit managers to effectively provide tailored and exceptionally individualized services through innovation, allowing them to attain a new competitive edge in a changed global market.
The platform achieves these objectives by offering many functionalities, including regulatory compliance solutions, clinical management programs, business intelligence tools, and implementation guidance.
Providers
FACETS enables healthcare providers, including hospitals, physician practices, and health systems, to integrate, streamline, and improve the effectiveness of patient care. It provides operational, technological, and consulting services to support virtual health's launch, progression, or improvement.
FACETS achieves this by adopting Artificial Intelligence and Analytics, Intelligent Process Automation, Security, and Cloud Infrastructure Services.
What FACETS aims to provide to the healthcare industry
- FACETS streamlines the member enrollment process, managing the details of individuals covered by health plans. It ensures accuracy in eligibility checks, enrollment data, and member information, facilitating a smooth and efficient enrollment experience.
- The platform is designed to handle the intricacies of benefits administration within health insurance plans. This includes managing different benefit packages and coverage details and ensuring that members receive accurate information about their healthcare benefits.
- One of the core features of FACETS is its robust claims processing capability. It manages the entire lifecycle of a healthcare claim, from submission to adjudication, ensuring accuracy, compliance with regulations, and timely reimbursement for healthcare services provided.
- FACETS assists in managing provider networks, helping healthcare payers maintain accurate and up-to-date information about healthcare providers. This includes details about participating providers, their specialties, and negotiated reimbursement rates.
Now, we shall discuss the four key feature areas of the FACETS platform. We shall discuss each of these, as well as what they involve, below:
Market vision
- Help to simplify the management risk
- Real-time integration enables value-based partnerships, risk adjustment, and quality enhancement.
- Maintaining compliance with changing rules and security standards
- Providing more flexible payment choices and risk stratification
Intelligent operations
- FACETS incorporates automation to streamline routine administrative tasks, reducing manual effort.
- The platform often includes robust analytics capabilities, leveraging data to provide insights into operational performance. Analytics tools within FACETS enable organizations to make informed decisions, optimize processes, and identify areas for improvement.
- This real-time functionality enhances the speed and accuracy of decision-making during patient encounters.
- Plans are automatically renewed to decrease administrative work.
- Dashboards that display essential information improve user productivity.
Optimized experience
- Enhance customer service and minimize batch operations using Billing 360 and Real-Time Billing functionalities.
- Leveraging Benefit 360 with a real-time Benefit Summary and information on members’ benefit usage
- Enhancing user experience through optimizing simple navigation, tailored content customization, providing personalized and adjustable workspaces to enhance productivity, and implementing an enhanced search functionality.
Enabled Enterprise
- Third-party integration of the FACETS solution
- The objective is to share data among TriZetto Healthcare Products to coordinate the entire company, eliminate duplicate data, and minimize timing discrepancies between systems.
- Store data on the cloud, either on Cognizant's private cloud or a preferred public cloud.
- Machine learning and artificial intelligence analyze core processing and provide timely decision-making insights.
- Enable the implementation of automation that utilizes the timely dissemination of data.
Real-world examples of FACETS in the healthcare industry
We have included two concise and practical case studies below to provide a more comprehensive understanding of FACETS in healthcare. This highlights the utilization of this IT platform by two prominent organizations in the healthcare sector and its implications for their customers.
Achieving strategic growth objectives
Geisinger Health Plan (GHP) sought to expand its market share and diversify its product lines. Nevertheless, due to the use of a 20-year-old core administration system, their outdated technology could not support their advanced commercial development strategy.
Through the utilization of the FACETS core system, GHP accomplished the following:
- Enhanced assistance for meeting regulatory requirements and addressing external market expectations
- An efficient and optimized process
- Enhanced automation
- An increase in errors
- Processes and systems is a long-term strategic goals, including participation in programs such as Health Information Exchanges
The auto-adjudication rates had a 10% increase, rising from 75% to 85%. GHP successfully attained a 100% rate of submitting documents to the Centers for Medicare & Medicaid Services within the designated timeframe. Additionally, GHP achieved a 99% accuracy in making payments to healthcare providers.
Find a course provider to learn Facets Business Analyst
Java training | J2EE training | J2EE Jboss training | Apache JMeter trainingTake the next step towards your professional goals in Facets Business Analyst
Don't hesitate to talk with our course advisor right now
Receive a call
Contact NowMake a call
+1-732-338-7323Enroll for the next batch
Facets Business Analyst Training Course Program
- Dec 15 2025
- Online
Facets Business Analyst Training Course Program
- Dec 16 2025
- Online
Facets Business Analyst Training Course Program
- Dec 17 2025
- Online
Facets Business Analyst Training Course Program
- Dec 18 2025
- Online
Facets Business Analyst Training Course Program
- Dec 19 2025
- Online
Related blogs on Facets Business Analyst to learn more

Business Analysts: The axis power of any business organization
In any organization, a Business Analyst is key personnel who ensures that operations tread forward smoothly without hiccups. Their job profile is to focus on specific business processes and ensure that the goals and milestones attached to it are achi

All You Need To Know Before Deciding To Become A Facets Business Analyst
Facets can be classified as comprehensive, scalable, flexible, enterprise-wide, production-proven core administration solutions meant for healthcare providers. Well, Facets offer a functionally rich modules set which allow providers to meet their bus
Latest blogs on technology to explore
From Student to AI Pro: What Does Prompt Engineering Entail and How Do You Start?
Explore the growing field of prompt engineering, a vital skill for AI enthusiasts. Learn how to craft optimized prompts for tools like ChatGPT and Gemini, and discover the career opportunities and skills needed to succeed in this fast-evolving indust

How Security Classification Guides Strengthen Data Protection in Modern Cybersecurity
A Security Classification Guide (SCG) defines data protection standards, ensuring sensitive information is handled securely across all levels. By outlining confidentiality, access controls, and declassification procedures, SCGs strengthen cybersecuri

Artificial Intelligence – A Growing Field of Study for Modern Learners
Artificial Intelligence is becoming a top study choice due to high job demand and future scope. This blog explains key subjects, career opportunities, and a simple AI study roadmap to help beginners start learning and build a strong career in the AI
Java in 2026: Why This ‘Old’ Language Is Still Your Golden Ticket to a Tech Career (And Where to Learn It!
Think Java is old news? Think again! 90% of Fortune 500 companies (yes, including Google, Amazon, and Netflix) run on Java (Oracle, 2025). From Android apps to banking systems, Java is the backbone of tech—and Sulekha IT Services is your fast track t
From Student to AI Pro: What Does Prompt Engineering Entail and How Do You Start?
Learn what prompt engineering is, why it matters, and how students and professionals can start mastering AI tools like ChatGPT, Gemini, and Copilot.

Cyber Security in 2025: The Golden Ticket to a Future-Proof Career
Cyber security jobs are growing 35% faster than any other tech field (U.S. Bureau of Labor Statistics, 2024)—and the average salary is $100,000+ per year! In a world where data breaches cost businesses $4.45 million on average (IBM, 2024), cyber secu

SAP SD in 2025: Your Ticket to a High-Flying IT Career
In the fast-paced world of IT and enterprise software, SAP SD (Sales and Distribution) is the secret sauce that keeps businesses running smoothly. Whether it’s managing customer orders, pricing, shipping, or billing, SAP SD is the backbone of sales o

SAP FICO in 2025: Salary, Jobs & How to Get Certified
AP FICO professionals earn $90,000–$130,000/year in the USA and Canada—and demand is skyrocketing! If you’re eyeing a future-proof IT career, SAP FICO (Financial Accounting & Controlling) is your golden ticket. But where do you start? Sulekha IT Serv

Train Like an AI Engineer: The Smartest Career Move You’ll Make This Year!
Why AI Engineering Is the Hottest Skillset Right Now From self-driving cars to chatbots that sound eerily human, Artificial Intelligence is no longer science fiction — it’s the backbone of modern tech. And guess what? Companies across the USA and Can
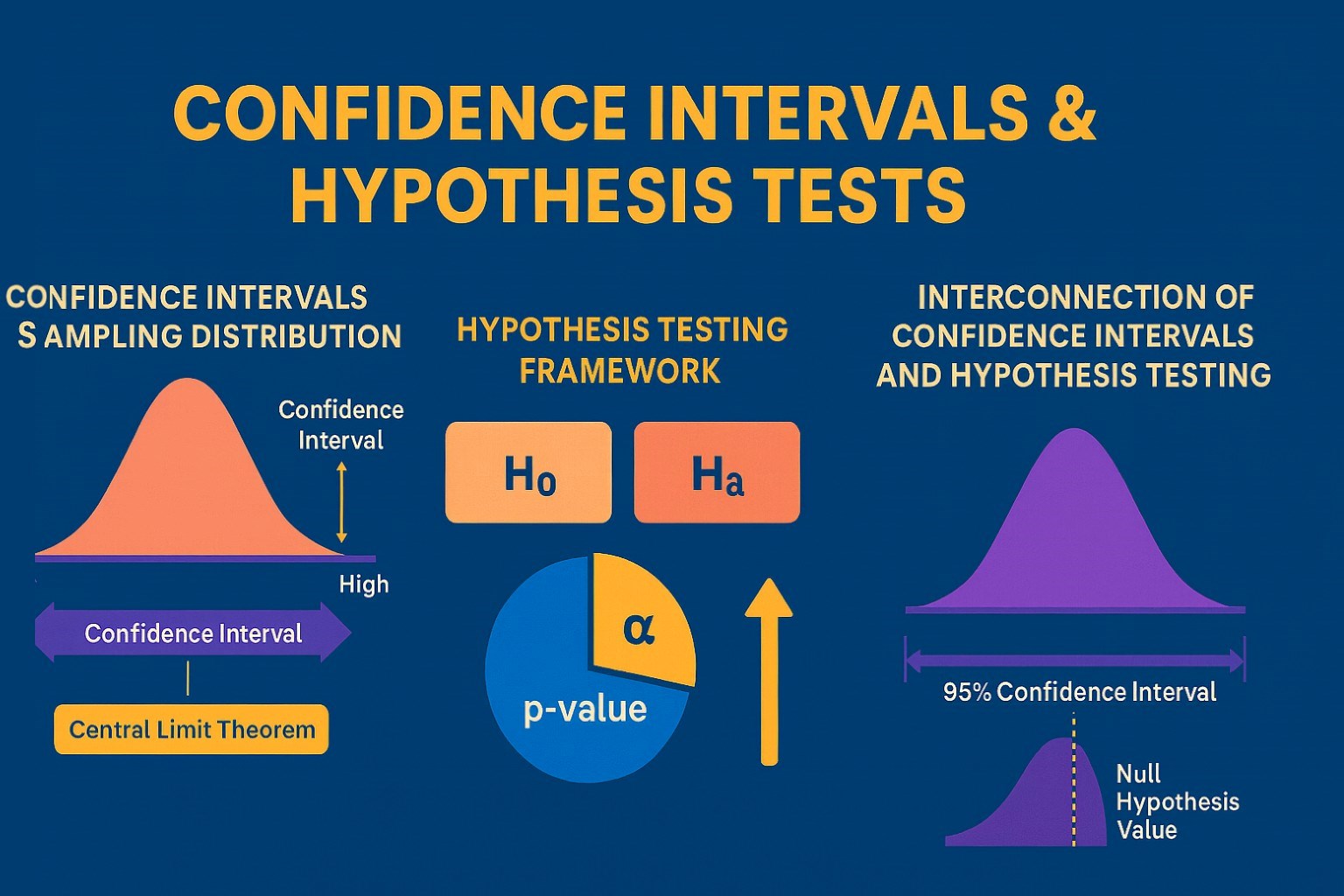
Confidence Intervals & Hypothesis Tests: The Data Science Path to Generalization
Learn how confidence intervals and hypothesis tests turn sample data into reliable population insights in data science. Understand CLT, p-values, and significance to generalize results, quantify uncertainty, and make evidence-based decisions.